The brain’s power generators, mitochondria, could hold the key to Alzheimer’s disease. Understanding them better is also shedding light on the potential of diabetes drugs in treating Alzheimer’s.
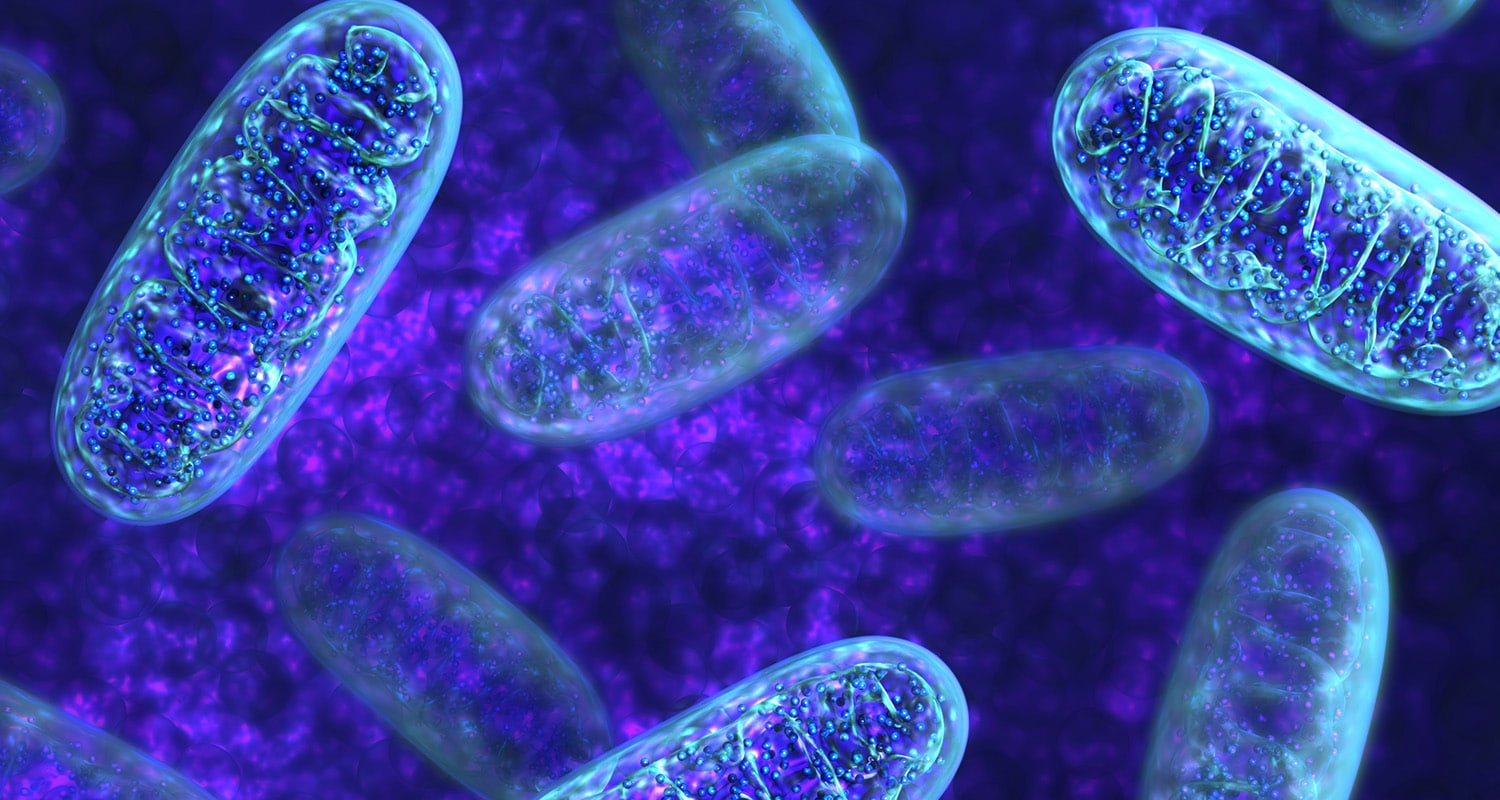
Despite accounting for just two percent of our body weight, the brain consumes 20 percent of the body’s energy. Driving energy production to fuel the brain are our mitochondria: factories within brain cells that convert oxygen and glucose fuel into energy. This process is called bioenergetics, and it is crucial for keeping brain cells healthy.
But, as we age, these brain energy factories begin to break down. The breakdown of mitochondria cells occurs alongside normal cognitive aging, but it is also linked to neurodegenerative diseases like Alzheimer’s.
Drugmakers developed an Alzheimer’s treatment called dimebon designed to target mitochondria, but the drug failed in trials. So far, there haven’t been any successful new experimental drugs that target this pathway. However, scientists haven’t given up on exploring the relationship between mitochondria and neurodegeneration — and their potential role in its treatment.
Could mitochondria dysfunction contribute to Alzheimer’s?
A powerhouse can get overloaded when there is too much electricity flowing through it. A similar dynamic occurs in the brain: Proteins that build up in the brain, and may lead to diseases like Alzheimer’s, called beta-amyloid plaques, can lead to dysfunctional levels of calcium, which leads to dramatic energy shortages in the brain and cell death.
In addition, the mitochondria in Alzheimer’s aren’t well-distributed inside of nerve cells. That means areas inside the neuron that perform more work don’t get nearly enough energy. Their physical structure and size differ from mitochondria in healthy brains. This might further accelerate the cell death which occurs in Alzheimer’s disease.
What might cause mitochondrial dysfunction in the first place? Changes in the blood vessels that bring oxygen to the brain affect the amount of oxygen — fuel for generating energy — that reaches mitochondria in the brain.
Insulin resistance, a condition associated with diabetes, is another risk factor for Alzheimer’s that contributes to mitochondrial dysfunction. In the brain, there is a reduction in insulin levels making it more difficult for cells to take up glucose and turn it into energy. There is already evidence from studies of obese and pre-diabetic adolescents that administering insulin improves cognition.
What can mitochondria tell us about the future of Alzheimer’s treatments?
Keeping mitochondria healthy directly or indirectly could be key for managing Alzheimer’s disease. While the drug dimebon failed, there may be drugs for other conditions that could help keep the mitochondria healthy.
The link between diabetes, insulin, and Alzheimer’s is well-documented. As insulin and other hormones that regulate glucose levels affect mitochondria and energy production, they are being investigated as Alzheimer’s therapeutics.
In a mouse model of Alzheimer’s, an insulin nasal spray could counteract some memory and cognitive dysfunctions however it did not translate so well to humans. A drug used to treat type 2 diabetes — liraglutide — is currently in Phase II trials for Alzheimer’s. It works by mimicking a protein that signals we’re full in the brain, glucagon-like peptide-1. Glucagon-like peptide-1 also controls energy flux in supportive brain cells called astrocytes and helps mitochondria stay healthy.
It may still be a few years until we find out if liraglutide works and how it affects mitochondria in the brain. For now, lifestyle changes, like eating the Mediterranean diet and getting enough exercise, are valuable preventative measures for Alzheimer’s — measures that also help make sure our brain cells have the power to help stave off the onset of the disease.













