Amyloid plaques are a hallmark of Alzheimer’s disease. The interesting thing is, not everyone who develops these plaques gets Alzheimer’s. Answering this question could reveal new clues about the underlying cause of the disease.
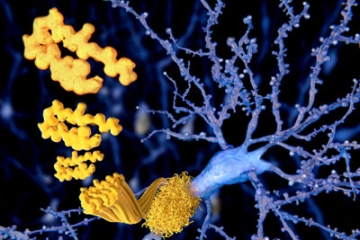
Scientists don’t know what causes Alzheimer’s. But the brain’s of everyone with Alzheimer’s do share a hallmark: clumps of toxic beta-amyloid plaques. This finding led to the development of the amyloid hypothesis: The idea that these plaques are responsible for cognitive decline and that clearing them could treat the disease. But there’s something that keeps baffling researchers — not everyone with amyloid plaques develops Alzheimer’s.
In a study published in JAMA Neurology in 2018, researchers assessed how many cognitively healthy older individuals had the toxic plaque in their brains. Out of 1,671 cognitively healthy people aged 80 to 89, about 43 percent were found to be “amyloid positive.”
While the plaques may precede cognitive decline, many of the people in the study with amyloid plaques did not develop cognitive impairment or Alzheimer’s disease. However, these cognitively healthy adults with amyloid positivity, the study found, were twice as likely to develop a form of mild cognitive impairment.
But scientists are still perplexed about the function of these beta-amyloid proteins and their role in cognitive decline.
Is Beta Amyloid Linked to Cognitive Impairment?
Until very recently, most Alzheimer’s drugs failed in clinical trials because they didn’t improve cognitive symptoms, even though they cleared out these plaques. The anti-amyloid drug Aduhelm recently received approval, but the clinical trials showed mixed results in its ability to slow cognitive decline.
Eisai’s anti-amyloid drug, Leqembi, however, is restoring some optimism in the approach. The drug recently received FDA approval through the accelerated pathway and published results from their Phase 3 trial suggesting that clearing plaques lead to improvements in cognition over 18 months.
Other researchers showed compelling links between beta-amyloid and other risk factors for Alzheimer’s disease and dementia. One study of cognitively healthy adults found that even one night of sleep deprivation resulted in increased beta-amyloid plaques in the brain.
Unfortunately, the accumulated evidence so far doesn’t have a simple definitive answer. Beta-amyloid might be involved or even cause cognitive impairment in Alzheimer’s disease, but it could also simply be a marker of something else that’s gone wrong in the brain. Some theorize it may even be part of the body’s response to fighting the disease.
Early Diagnosis Could Answer the Question
By the time Alzheimer’s is diagnosed, it may be 10 to 20 years after the first pathological changes in the brain appear. Since beta-amyloid is difficult and expensive to measure, scientists are looking for other biomarkers in the blood and brain (via measuring the brain’s electrical activity). This may make it easier to detect other important risk factors for the disease, before symptoms arise.
By the time a person is diagnosed, it may be too late to stop the downstream effects of beta-amyloid plaques. With early diagnosis, it may thus be easier to develop better treatments for Alzheimer’s and identify the biomarkers most closely linked to cognitive impairment.












